Pilonidal Cyst
Can Pilonidal Cysts Cause Sciatica
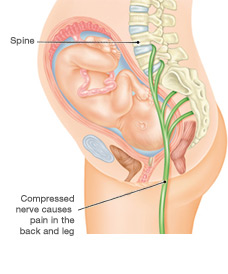
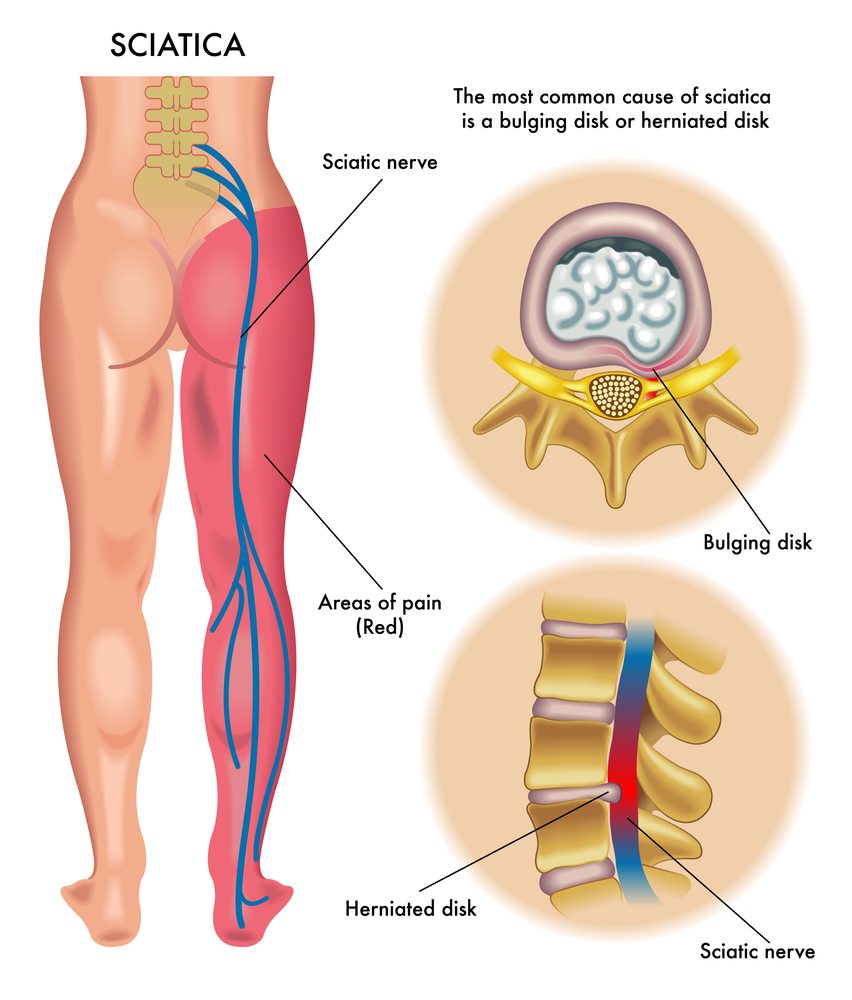
Sciatica is a condition that causes sciatic nerve pain, numbness, and tingling in the leg or feet. It can be caused by many different things, such as cysts. This article will explore whether sciatica symptoms are related to pilonidal cysts.
Read more about Can Pilonidal Cysts Cause Sciatica
 We’ll discuss what sciatica is, what causes it, and whether or not pilonidal cysts contribute to sciatic pain.
We’ll discuss what sciatica is, what causes it, and whether or not pilonidal cysts contribute to sciatic pain.
More about Can Pilonidal Cysts Cause Sciatica

Does Pilonidal Cyst Cause Sciatic Nerve Pain?
Pilonidal cysts are sacs of tissue that contain air or fluid. Cysts like this one commonly develop along the crease of the buttocks. An infection of the skin generally causes pilonidal cysts. As for sciatica, this condition refers to nerve pain originating from your buttock/gluteal area, usually due to an injury or irritation to this nerve.
Although both conditions are located on the buttocks, pilonidal cysts do not cause sciatic pain.
Sciatica is mainly related to the human anatomy’s musculoskeletal system, while pilonidal cysts have more to do with the integumentary system.
Diseases and disorders that usually cause sciatica are correlated to musculoskeletal disorders and neurological disorders.
Both sciatica and pilonidal cysts affect the lower limb anatomy, and the symptom of pain is present in both cases but diagnosis greatly differs.
A pilonidal cyst causes chronic pain due to dead skin and hair trapped in the area of the buttocks. Sitting down can be extremely painful when a pilonidal cyst is present.
Sciatica, on the other hand, is caused by irritation of the sciatic nerve. The leg and lower back are usually the most painful if a person has sciatica. Sciatic pain can often be felt after prolonged sitting or standing.
What Cyst Can Cause Sciatica?
Perineural cysts
A perineural cyst, also known as a Tarlov cyst, is a fluid-filled sac that forms on the nerve root sheath, usually in the sacral area of the spine. Other parts of the spine can also be affected.
A person with a perineural cyst may not have any signs or symptoms. They are usually not noticed by the person who has them. The cysts only become symptomatic when they fill with spinal fluid and increase in size. As a result, the cysts may compress nerves and cause other problems.
Pain is one of the most common symptoms associated with perineural cysts. Enlargement of the cysts can compress the sciatic nerve, which can result in sciatica.
Synovial cysts
A synovial cyst is a small, fluid-filled lump that develops on the lower part of the spine. Cysts of this type are not cancerous and often do not cause symptoms. Unfortunately, they can sometimes result in problems like sciatica.
The synovium lines the inside surface of joints. In addition to lubricating and protecting joints, synovial membranes also produce synovial fluids. Sometimes, synovial cysts develop from the buildup of fluid within the membrane.
Older adults and people with joint conditions such as arthritis are more likely to develop synovial cysts.
One or more of the following symptoms may accompany synovial cysts: back pain, experience pain in the legs, difficulty walking or standing, numbness, or tingling.
What Conditions Can Cause Irritation of the Sciatic?
Piriformis syndrome
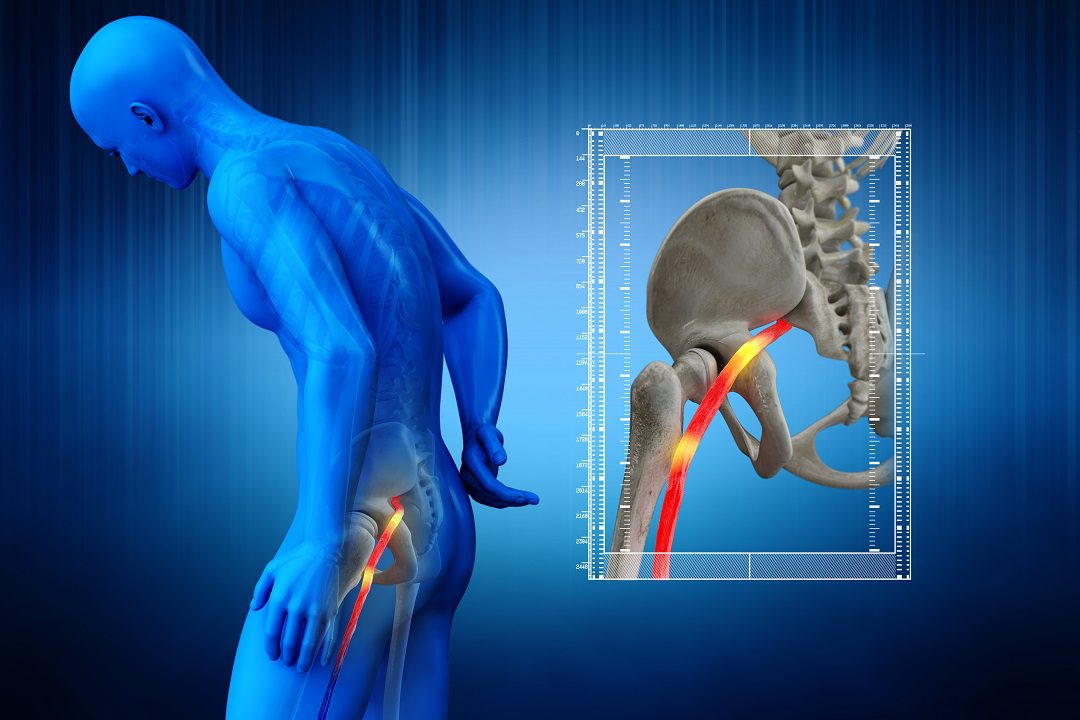
Piriformis syndrome refers to a painful condition that occurs when the piriformis muscle spasms. The piriformis muscle can also irritate the sciatic nerve. When the sciatic nerve is upset because of the piriformis muscle, it can cause pain, numbness, and tingling down the back of the leg and even into the foot.
In the buttocks, near the top of the hip joint, is a flat, band-like muscle called the piriformis. The hip joint and thigh are stabilized by this muscle, which lifts and rotates the thigh from the body.
The symptoms of Piriformis syndrome usually begin with pain, tingling, or numbness in the buttocks. It is possible to experience acute pain along the length of the sciatic nerve.
When the piriformis muscle compresses your sciatic nerve, the result is excruciating pain. It is also possible to experience pain while climbing stairs, applying firm pressure directly over the piriformis muscle, or when sitting for long periods.
However, most cases of sciatica are not caused by piriformis syndrome.
Spondylolisthesis
Spondylolisthesis is a condition wherein there is instability in the spine. This instability is due to the vertebrae moving more than they should. A vertebra slips out of place and can cause pressure on a nerve, resulting in lower back pain or leg pain.
Many factors can cause the vertebrae to slip out of place. When the vertebra is out of place, it puts pressure on the bone below it.
Symptoms do not usually accompany spondylolisthesis. If leg pain is felt, it can be due to the compression or a “pinching” of the nerve roots that exit the spinal canal.
By slipping out of place, the vertebrae compress or pinch the nerves, narrowing the space needed for them.
Osteoarthritis
Gradual deterioration of your joints’ cartilage leads to osteoarthritis. Cartilage is a firm, slippery tissue that facilitates joint motion without friction.
Osteoarthritis can affect any joint. However, the condition is most common in your hands, knees, hips, and spine. It is also a prevalent cause of pinched nerve or sciatica pain.
Aside from sciatica, osteoarthritis can also cause stiffness and swelling. In some cases, it can also cause reduced function and disability; some people may not be able to do the things they usually do.
How Can You Manage Sciatica Pain?
Sciatica can often be treated at home in a few weeks. Typically, your doctor will recommend trying some combination of solutions for pains that are relatively mild and aren’t preventing you from doing your everyday activities.
In addition to teaching you stretching and exercise routines, physical therapists can help improve your posture, which will relieve the strain on the sciatic nerve.
Stretches for the lower back can help alleviate sciatica pain. Moving around can help reduce inflammation, so taking a short walk can be beneficial.
You can also try aspirin, ibuprofen, and naproxen. However, do not use them for an extended period without consulting your doctor. A stronger muscle relaxant or anti-inflammatories might be prescribed by your doctor if over-the-counter remedies do not work.
In about 5-10% of sciatica cases, surgery is the only option left. Your doctor may recommend surgery if you have mild sciatica but are still in pain after 3 months of resting, stretching, and taking medicine.
A rare but serious complication of sciatica is cauda equine syndrome, in which your bladder and bowels become impaired. In that case, surgery is the only option.
How serious is a pilonidal cyst?
It is not dangerous, but pilonidal cyst can turn into an infection, so it should be treated. A pilonidal cyst that becomes infected forms an abscess that drains pus through a sinus. Pain, a foul smell, and bleeding are common symptoms associated with the abscess of pilonidal cyst.
The most common complication of pilonidal cysts is the recurrence of the abscess. A systemic infection is also possible.
Will a pilonidal cyst go away on its own?
Minor surgery is one way of getting rid of a pilonidal cyst.
It is possible for pilonidal cysts to drain and disappear by themselves. A pilonidal cyst may cause you to have recurring symptoms over time.
To get rid of a pilonidal cyst at home, the affected area should be treated daily by applying a warm, wet compress. It will help drain the cyst by pulling out the pus. Pain and itching can be relieved in this way.
A warm, shallow bath may also be helpful. Ibuprofen or other pain relievers can be taken if your cyst hurts.
Why does my pilonidal cyst keep coming back?
Patients sometimes have more than one sinus tract when first operated on for pilonidal cyst, but the second one is not detected. A period of time may pass before that tract begins to cause problems, requiring another surgery.
Other times, the patient acquires another instance of pilonidal disease after the first one. The same factors that led to the first case could contribute to an additional chance of pilonidal cysts, which will result in hair penetrating the skin in the buttocks area.
Excision procedures don’t always completely heal; thus, you may still experience the problems associated with your pilonidal sinus long after your initial surgery.
If an incision scar grows near the cyst, the cyst may return because the area becomes infected again.
How Can I Prevent Pilonidal Cyst From Coming Back?
Select the Best Treatment
Various treatments for chronic pilonidal sinuses have different success rates over time. By choosing the best treatment prescribed by your doctor for your specific case, you might help protect yourself.
Exercise More
Maintaining an active lifestyle not only boosts your health but it can help reduce pressure on your buttock cleft. By doing this, fewer hairs may make their way under the skin.
Furthermore, an active lifestyle can help you lose weight. Weight loss can reduce your risk of developing pilonidal sinuses when you are overweight or obese.
Remove Hair
You may be advised to reduce hair in your buttocks area if you have body hair in that area. Pilonidal sinuses can often develop in people with a lot of body hair.
It is sometimes recommended to use shaving cream and depilatory lotions to remove hair. The use of lasers for hair removal is another good choice.
Follow Doctor’s Advice
Follow your doctor’s post-care management regardless of the type of treatment options you had for pilonidal disease. A surgical infection may occur if you do not follow their medical advice.
Cleanse and keep wounds dry at all times. During the healing process, it is necessary to pack the open surgical site regularly.
Pilonidal cysts are a round sac of tissue that’s filled with air or fluid. This common type of cyst is located in the crease of the buttocks and is usually caused by a skin infection. More than 70,000 cases reported in the U.S. every year. Men are three to four times more likely to be diagnosed with a pilonidal cyst than women. A pilonidal cyst is a non-contagious skin condition – you can’t spread it (just like a pimple) It’s caused by ingrown hairs found in the crease of the buttocks causing a skin infection.
If you have a pilonidial cyst, your provider may spot what looks like a pimple or oozing cyst. They may also ask you several questions, including: Has the cyst changed in appearance? Is it draining any fluid? Do you have any other symptoms? Very rarely, your doctor will be able to tell you if you have an abscess or a sinus cavity.
If you have a pilonidal cyst, you may or may not need surgery to remove it. There are several other treatment options besides surgery for the cyst. Antibiotics can treat skin inflammation, but antibiotics can’t heal pilonidial cysts on their own. Laser therapy can remove hair which otherwise might become ingrown and cause more cysts to come back. A pilonidal cyst is not life-threatening, but it can pose several long-term health risks.
Losing weight (if you are currently overweight) and avoiding sitting for too long can lower your risk. Shaving the hair around your buttocks once a week or more can help prevent ingrown hairs. If you have a pilonidial cyst, you may need to take some time off of work if you develop symptoms. Perineural cysts are often misdiagnosed because they rarely cause symptoms. When they do cause symptoms, one of the most common is pain in the lower back, buttocks, or legs.
This occurs when the cysts become enlarged with spinal fluid and press on nerves. In rare cases, cysts that cause symptoms and are not treated will cause permanent damage to the nervous system. The cysts can be drained to provide temporary relief of symptoms. Only surgery can keep them from refilling with fluid and producing symptoms again. Most people with perineural cysts will never have any symptoms or need any treatment.
If you have symptoms, they may need treatment to relieve pressure and discomfort. Surgery to remove the cysts is a dangerous procedure that carries significant risks. Only 1 percent of people with these cysts experience symptoms. The only permanent treatment for them is to have them surgically removed.
- Pilonidal Cyst A pilonidal cyst is a round sac of tissue that’s filled with air or fluid.
- This common type of tarlov cyst is located in the crease of the buttocks and is usually caused by a skin infection.
- Pilonidal cysts are a common condition, with more than 70,000 cases reported in the U.S. every year.
- This common type of cyst is located in the crease of the buttocks and is usually caused by a skin infection.
- Pilonidal cysts can cause pain and need to be treated.
- Is a pilonidal cyst contagious?
- A pilonidal cyst is a non-contagious skin condition – you can’t spread it (just like a pimple).
- There are several steps you can take to help prevent getting pilonidal cysts or to keep them from coming back.
- These steps include: Regularly washing and drying your buttocks (to keep the area clean).
- OUTLOOK / PROGNOSIS Is a pilonidal cyst fatal?
- A pilonidal cyst is not fatal in itself.
- This occurs in rare cases when the cysts become enlarged with spinal fluid and press on nerves.
- Symptoms of perineural cysts People with perineural cysts are not likely to have any symptoms.
- Diagnosis of perineural cysts Because most perineural cysts cause no symptoms, they are typically never diagnosed.
- Your doctor can order imaging tests to identify them if you have symptoms.
- A CT scan with a dye injected into the spine can show if fluid is moving from the spine into cysts in the sacrum.
- Treatments for perineural cysts For most cases of perineural cysts, no treatment is needed.
- The only permanent treatment for perineural cysts is to have them surgically removed.
- Surgery is usually recommended for serious, chronic pain, as well as bladder problems from the cysts.
Related searches