¿Alguna vez ha sentido una sensación de ardor o descargas eléctricas en la parte baja de la espalda y luego en las piernas? Si es así,...


Have you ever felt a burning sensation or electric shocks down your lower back and then into your legs? If so, don’t worry, you are not...
Para muchas personas que sufren de ciática, el dolor puede ser debilitante. Afortunadamente, varios tratamientos disponibles pueden ayudar a aliviar el dolor, incluidos medicamentos de venta...
Correr es una excelente manera de hacer ejercicio y mejorar su estado físico general, pero también puede ser riesgoso si tiene ciática. La ciática es una...
Running is a great way to get exercise and improve your overall fitness, but it can also be risky if you have sciatica. Sciatica is a...
Para muchas personas, la ciática es una condición temporal que desaparece. Sin embargo, para algunas personas, la ciática puede ser una condición crónica que dura meses...
Para muchos practicantes de yoga, la ‘postura de la paloma’ es una flexión hacia atrás muy querida. Para las personas que luchan contra la ciática, puede...
Si alguna vez ha tenido dolor en los nervios que le bajan por las piernas y la parte baja de la espalda, entonces conoce la agonía...
If you have ever had nerve pain shooting down your legs and lower back, then you know the agony of sciatica. It’s not something to be...
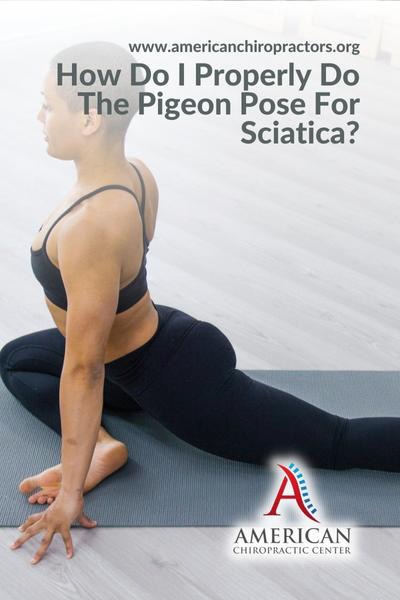
For many yoga practitioners, the ‘pigeon pose’ is a beloved backbend. For individuals struggling with sciatica, it can be hard to even imagine ever being able...