What are the best creams for back pain? When aches and pains become an obstacle to living a fulfilling life, you should consider applying a pain...
Do Chiropractors Help With Sciatica Nerve Pain? Chiropractors are experts in many fields. They offer relief for chronic pain, car accident injuries, and other ailments. Can...
How Your Sciatica Nerve Can Cause Abdominal Pain A person may experience abdominal pain due to sciatica, which is caused by the compression of a nerve...

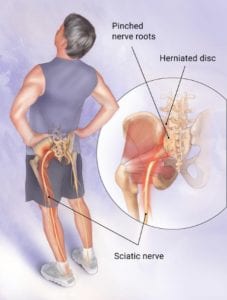
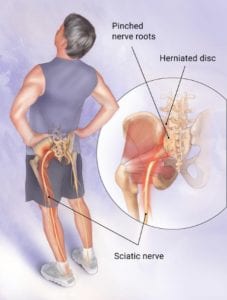
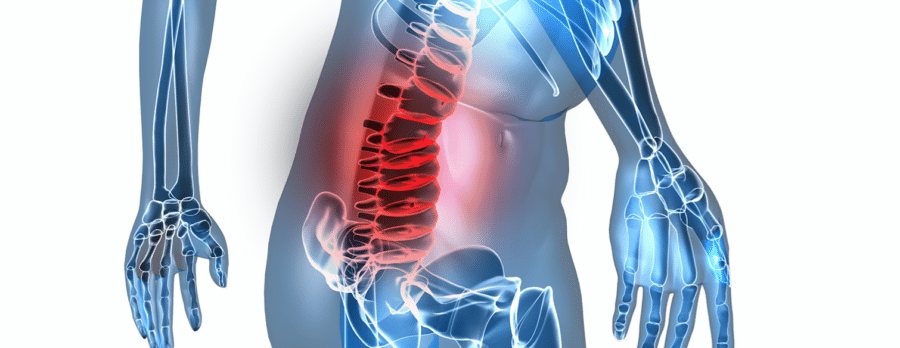
What is sciatica? Sciatica is a pain that shoots down the leg, caused by pressure on the sciatic nerve. It’s no surprise that sciatica patients often...
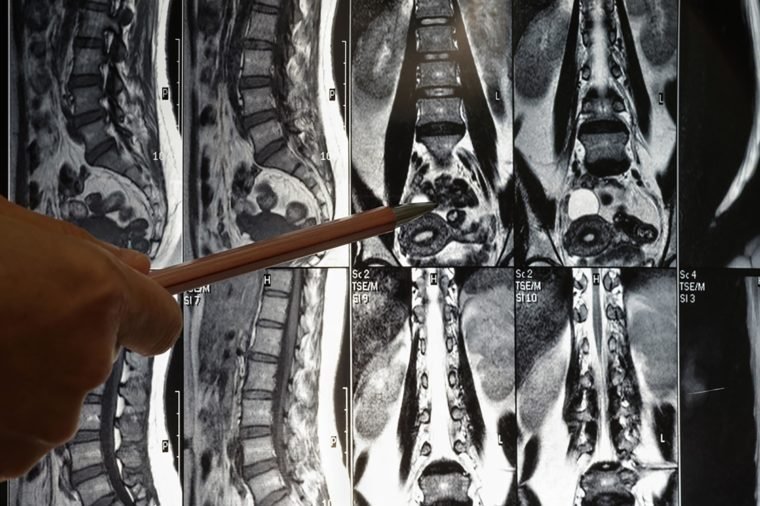
Sciatica is a condition that causes sciatic nerve pain, numbness, and tingling in the leg or feet. It can be caused by many different things, such...
Oh, the agony! One minute, you’re bopping around like a kangaroo and the next, your knee is howling like a banshee. Is it just a creaky...
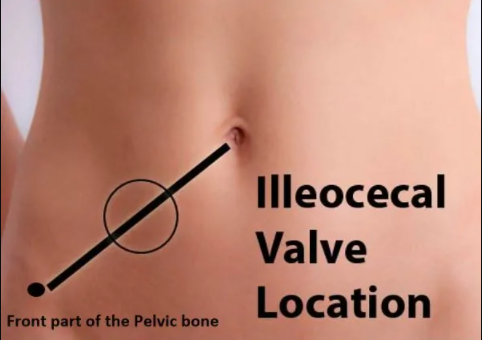
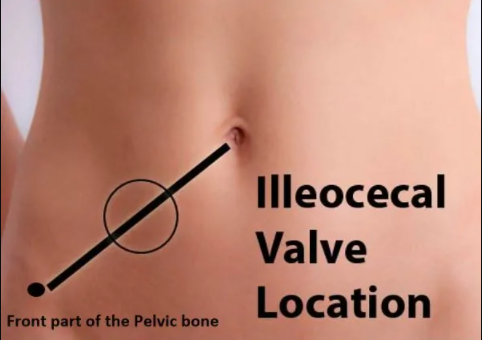
So you think you may have Ileocecal valve syndrome? Ileocecal valve syndrome may cause constipation and digestive problems. Constipation can lead to colitis, diverticulosis, and other...

So you are looking to relieve sciatic nerve pain? You can relieve sciatica pain permanently with heat packs, stretching and strengthening the lower back, utilizing over the counter...


Exercise is one of the most effective strategies to alleviate the symptoms of sciatica and provide pain relief. However, the manner in which you exercise is...

Five of the best anxiety CBD oils Is CBD legally binding? CBD products derived from hemp with feederally legally legalized but are still illegal in accordance...