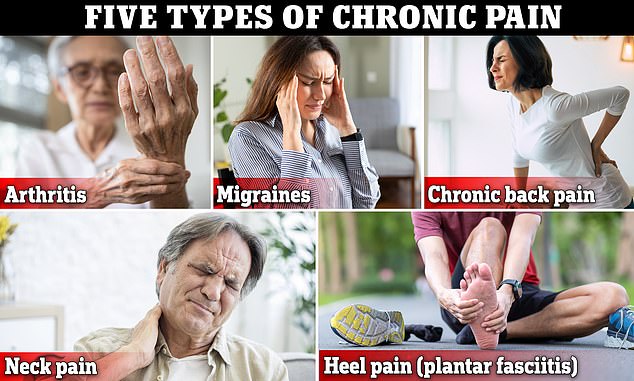
New CDC studies show that one of FIVE Americans suffer from chronic pain. Here’s how you can do without resorting to prescription medications.
-
Between 20 to 22 percent of Americans suffer from chronic painful, crippling pain
-
Women, divorced individuals and those in poor health were the ones to suffer most severely
-
The opioid crisis is in full swing, doctors suggest non-drug alternatives
An alarming 21 % of Americans suffer from chronic pain, a broad term that covers a variety of debilitating ailments.
More than one-in-five Americans suffered from chronic pain between 2019 and 2021, according to new information of the Centers for Disease Control and Prevention (CDC) illustrates.
Doctors have numerous instruments in their arsenal to treat ailments that result in chronic, severe pain for example, chronic back pain or frequent migraines. One of these options is opioid painkillers that are effective but carry significant danger of addiction.
The introduction of prescription opioids that induce euphoria has led to a steady trend of a zealous prescription by profit-driven doctors and drug companies. At one time the prescription of opioids topped the 81st percentile for each 100 people.
The current standard of care has changed to include non-pharmaceutical remedies to treat pain, as an alternative to the risky medication. DailyMail.com dissected several of these options to treat some of the most prevalent reasons for chronic pain that cause life-threatening damage.
Between the years 2019 and 2021 the incidence of chronic pain in American adults ranged from 20 percnet to almost 22 percent. The rate of chronic pain that is high-impact was ranging from 7 percent to 8 percent.
The latest report from the CDC published on Thursday estimated that 51.5 million adults live suffering from chronic pain. Of the majority, 17.1 experienced what could be described as high-impact chronic pain, which is defined as persistent pain that has also impacted working or daily activities for a majority of the time or even every day in the last three months.
The researchers used information from 2019 to 2021 to create an annual poll.
In comparison to the data collected from 2006, it is apparent the chronic pain issue is getting more prevalent. The CDC stated that at the time, 10% of people reported that their pain lasted for at least a year.
While CDC researchers didn’t provide a reason the reason why so many Americans suffer from discomfort, experts from outside have speculated on a myriad of causes.
The United States is facing a obesity problem, with 40 percent of Americans overweight and 70 percent obese. A poor diet is linked to chronic discomfort.
Experts believe that the lack of exercise and sedentary lifestyles embraced by the majority of Americans causes damage.
An University of Georgia study published in the year 2000 found that 75 % of Americans aren’t meeting minimum levels of physical activity.
A large portion of the population also eats diets comprised mostly of processed foods that are associated with poor overall health and chronic pain according to recent research, 13 percent of the population addicted to these chemical-rich foods.
The report provides insight into the amount of people who has been likely to be confronted by the idea of using prescription painkillers like oxycodone for their chronic pain.
But these drugs are infamously hazardous and pose a significant danger of addiction.
The number of fatal overdoses caused by opioids exceeded the number of 80,000 in 2021. This is about 70% of the total.
Chronic back pain
There are more than sixteen millions US adults – 8 per cent of all Americans – suffer from chronic back discomfort.
The condition can seriously hinder an individual’s life daily and cause a continuous pain, dull or and sharp pains.
It is also aggravated maybe in a way that is counterintuitive, by laying down too long.
This is because laying prone for a long period of time places stress onto the spine and may result in sore or stiff muscles.
Doctors advise against resting for longer than a couple of days and advise people to move.
Stretching is a great place to begin. Although it isn’t a panacea, yoga postures can be extremely effective in giving some temporary pain relief.
A yoga pose that is commonly used, called child’s pose is a stretch that stretches spinal extensors. These are muscles connected to the back of the spine that enable us to stand and lift things.
The pose can also help improve blood circulation.
The act of swimming, or any moderate water activity is considered to be extremely beneficial.
A report from 2009 by Turkish scientists that was published in Spine discovered that water-based exercises helped improve the condition of people with disabilities and improved health better than other types of exercises done outside of water.
The back pain could be aggravated by sitting too long, as sitting prone for a long period of time places stress on the spine
A meta-analysis from 2018 of eight research studies published within the American Journal of Physical Medicine & Rehabilitation concluded that ‘Aquatic exercise was statistically significant in reducing VAS scores [measure of the intensity of pain] and improved physical function.
These results suggest that aquatic exercise could play a impact on the quality of physical and emotional health living.’
In the end, experts suggest making some minor changes to the way you sleep as poor posture is widely known to trigger back discomfort.
Sleepers who prefer to sleep on their backs need to place a cushion under their knees. Side-sleepers must place a pillow between their knees in order to keep the spine in an upright position and ease the strain upon their back.
Arthritis
“Arthritis” is a term that generally refers more than 100 joint disorders which include the most prevalent forms, osteoarthritis and rheumatoid arthritis
Arthritis, a condition that is that is characterized by stiff, swollen joints that can the pain and discomfort that gets worse as we age, affects 60 million Americans.
The term “arthritis” generally means more than 100 joint disorders that include the most well-known forms, osteoarthritis and rheumatoid arthritis.
Osteoarthritis results in the break in cartilage, a hard tissue which covers the edges of bones, where they form joints. It’s often described as “wear and tear” arthritis.
The pain and discomfort it causes is due to years of deterioration of cartilage which can cause inflammation in joints that are frequently used including hips, knees and shoulders.
People suffering from pain could get physical therapy by a licensed professional experts say.
Physical therapy is a series of exercises designed to build muscles around joints, easing some of the strain on the bone and cartilage.
Therapists may employ equipment such as foam rollers to ease hip pain for patients suffering from hip osteoarthritis or resistance bands that have been found to aid patients ease arthritis pain in their knees.
A report for 2020 that was that was published by The New England Journal of Medicine discovered that osteoarthritis patients in their knees who were treated with physical therapy experienced lower levels of pain and functional impairment within a year than those receiving a glucocorticoid injection.
It is also believed that PT can assist in easing some of the pain that comes with rheumatoid joint, which is a condition which can cause your immune system become active, attacking healthy tissue such as joints of the spine hands, spine and feet.
The positive side is that government and private health insurance usually covers the costs of PT at a minimum when it is medically required.
Another type of physical therapy cannot be covered under insurance and can be very expensive.
It is expected that University of Southern California researchers will begin a study on the advantages of surfing for chronic pain.
In charge of the research is Dr. Jason Kutch, a professor at the USC Division of Biokinesiology and Physical Therapy and Physical Therapy. He discovered that his own chronic pain went away following his surfing sessions and that the pain he experienced during non-surf days was greatly decreased.
Numerous research studies also suggest alternative treatments that aren’t medication-based to treat Rheumatoid Arthritis.
One of them is acupuncture.
A needle that is properly placed produces an electrical signal that travels through the spinal cord to the brain, prompting the release of two forms of neurotransmitters known as endorphins and the enkephalins.
Researchers believe that the release of chemicals can help reduce the pain sensation.
Migraines
A cold compress or an ice pack, also referred to cold therapy – could be an effective way of treating pain
Migraines that are characterized by throbbing and pulse-like pain that begins deep within the brain and is centered around one region in the brain for an extended period of time, and usually gets worse in time. It’s more than a headache.
The condition is quite widespread with around 40 million Americans suffering from attacks.
Chronic migraine is a problem that affects smaller numbers of people – around 2 percent of the world population.
Migraines are deemed chronic when they occur at minimum 15 times per month for a period of three consecutive months.
Antiseizure medications and monoclonal antibodies or Botox shots are often the most effective treatment for migraines which can be painful and debilitating.
As well as aiding with pain relief for arthritis, Acupuncture has also aid migraine sufferers.
Acupuncturists strategically place needles on pressure points such as those in the neck and on the head which trigger the release of endorphins which stimulate the circulatory system, which is a large component of the treatment that helps to ease the pain of headaches.
Patients who are apprehensive about needles might want to avoid acupuncture, that can be a nerve-wracking experience.
In such a situation, they may opt for a mask that can block out light sources, since photosensitivity is a significant cause and manifestation for migraines.
An ice or cold pack – also referred to as cold therapy can be an effective option to treat the pain.
The cold may constrict blood vessels, a process known as vasoconstriction. It also helps to reduce pain neurotransmission to the brain.
A study from 2013 published in the Hawai’i Journal for Medicine and Health showed that, of 55 patients suffering from migraine, and received the frozen wrap for their necks for them to put on, 77% of them said the treatment eased some of their discomfort.
They were further asked “Did they need to take any medication to relieve your headache? half of the people who wore neck wraps frozen said yes, significantly lower than the 85 percent of non-frozen wrap users who also replied yes.
Neck Pain in the neck
If you are dealing with neck pain caused by muscle strain using gentle heat can assist.
Neck pain that is chronically due to muscle strain and nerve compression. Things like rapid and frequent weight lifting can result in strained muscles, particularly if you’re only using only one part of the body.
The compression of nerves, however, is when the nerves in the neck are squeezed or compressed as they disengage from the top spine which can cause extreme pain that can radiate into the armpits or shoulders.
If you are treating muscles strain, using gentle heat could aid.
Experts suggest covering a heat pad with a towel before placing it on your neck or sitting under an icy shower for couple of minutes to loosen up the tight muscles in your neck.
This, when followed by a relaxing massage can be very beneficial by relaxing muscles.
A pillow propped up under the neck to help keep it in a straight position has been proven to aid.
Memory foam pillows and latex specifically were found in a study from 2020 which was released in International Journal of Environmental Research and Public Health to aid in relieving neck discomfort than pillows made with cotton or feathers.
Experts advise those suffering from neck pain to opt for flat pillows. Tall pillows have been proven to increase tension on spine and neck. They also alter their curvature. This leads to pain and sleeping problems.
Heel pain
About one-in-10 people will be diagnosed with plantar fasciitis, a leading cause of heel pain at some point in their lives.
An ongoing stabbing pain in the heel can cause plantar fasciitis, one of the most frequently cited sources of pain in the heel. About one-in-10 individuals will suffer from plantar fasciitis at some point throughout their lives.
Plantar fasciitis occurs as a result of inflammation of the plantar fascia an attachment made of fibrous tissue that connects in the heels to the balls of the feet as well as the toes.
If the plantar fascia gets stretched out too much or is overused it could result in plantar fasciitis.
Patients suffering from plantar fasciitis should opt for comfortable, well-cushioned and supportive shoes or orthotic inserts.
The shoes should be firmly anchored in the sole, and cushioned in the midfoot area to protect the heel, the area with which pain is often associated with.
Stretching is also beneficial to many sufferers of plantar fasciitis. Physical therapists advise that this could be accomplished using a rolling ball or a water bottle back and forward beneath the foot to relieve pain, beginning below the foot’s ball and finishing just prior to the heel.
Heel raises may also help. Beginning with the balls of your feet on the edges of a bottom step, therapists suggest gradually and gently lowering the heels beneath the edges of the steps then slowly rising up to the balls of the feet.
There are some who may want to consider an overnight splint that can be worn at night or wearing a type of shoe cover and the ankle that keeps feet in an posture that gently stretch the plantar fascia as well as the muscles in the calf.
Applying ice to the region that is hurting every day for five to ten minutes each time will aid in treating plantar fasciitis, according to experts at NYU.